r/anhedonia
Personal Wiki
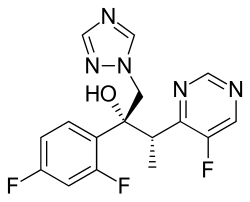
Voriconazole
- Pharmacological Actions
- Voriconazole's primary pharmacological action is the inhibition of fungal cytochrome P450 enzyme 14α-demethylase, a critical enzyme in the biosynthesis of ergosterol, a vital component of fungal cell membranes. This inhibition leads to the accumulation of 14α-methylated sterols and a decrease in ergosterol, altering cell membrane permeability and ultimately inhibiting fungal growth. Research indicates it is active against pathogens such as Aspergillus, Candida, Fusarium, Scedosporium, Exserohilum rostratum, Cryptococcus neoformans, and C. gattii, with variable activity against Fusarium and Scedosporium apiospermum.
- The effectiveness over time is concentration-dependent, with optimal therapeutic plasma concentrations typically maintained between 2 and 5 mcg/mL. Higher concentrations may lead to adverse effects, as discussed later.
- Half-life
- The elimination half-life of Voriconazole is approximately 6 hours for a 200 mg oral dose, based on studies in healthy adults. However, due to its non-linear pharmacokinetics, the half-life is dose-dependent, varying from 6 to 9 hours at steady state following multiple oral doses of 200 mg every 12 hours. This non-linearity is likely due to saturable hepatic metabolism, primarily via cytochrome P450 isoenzymes CYP2C19, CYP2C9, and CYP3A4, which can lead to dose-dependent accumulation.
- Bioavailabilities
- Oral Bioavailability: Approximately 96%, allowing for effective switching between IV and oral administration. Peak plasma concentrations are achieved within 1–2 hours, though food can reduce mean peak plasma concentrations by 34% and the extent of absorption by 24%, suggesting it should be taken on an empty stomach.
- Intravenous (IV) Bioavailability: 100%, as it is directly administered into the bloodstream, ensuring complete bioavailability.
- Dosages
- Dosages vary by condition, patient weight, and administration route. Below is a detailed breakdown for adults with invasive aspergillosis, a common indication:
Route Weight (kg) Loading Dose Maintenance Dose Maximum Dose Notes Oral ≥40 Not specified 200 mg every 12 hours 300 mg every 12 hours Increase if response inadequate, reduce by 50 mg steps if not tolerated. Oral <40 Not specified 100 mg every 12 hours 150 mg every 12 hours Adjust based on response and tolerance. IV All 6 mg/kg every 12 hours for 2 doses 4 mg/kg every 12 hours 4 mg/kg every 12 hours Reduce to 3 mg/kg if not tolerated; monitor for toxicity. - For other conditions such as candidemia or fungal infections caused by Scedosporium and Fusarium, dosages may differ, and specific guidelines should be consulted. Pediatric dosages also vary, typically based on body weight, with maximum oral doses up to 350 mg every 12 hours for certain age groups.
- Safe Range, Minimum Effective Dose, and Maximum Dose
- Safe Range: Research suggests maintaining serum trough concentrations between 2 and 5 mcg/mL is safe and effective. Concentrations above 5 mcg/mL are associated with increased risk of adverse effects, including neurotoxicity, visual disturbances, and liver toxicity.
- Minimum Effective Dose: While not explicitly defined, standard maintenance doses start at 100 mg every 12 hours orally for adults weighing less than 40 kg, indicating a likely minimum effective dose for many patients.
- Maximum Dose: For adults ≥40 kg, the maximum oral dose is 300 mg every 12 hours, and IV maintenance is up to 4 mg/kg every 12 hours, with reductions recommended if toxicity is observed.
- LD50 and Toxicity
- LD50: In animal studies, specifically rats, the oral LD50 is reported to be between 800 and 1600 mg/kg body weight. Human LD50 data is not available, as such values are typically derived from animal models and not directly applicable to humans due to ethical and practical constraints.
- Toxicity and Dangerous Dosage: Serum concentrations exceeding 5 mcg/mL are considered potentially dangerous, with risks including visual disturbances (e.g., photophobia, blurred vision), liver toxicity (elevated transaminases, jaundice), and severe skin reactions such as Stevens-Johnson syndrome and toxic epidermal necrolysis. Overdose symptoms may include prolonged QTc interval and other systemic toxicities, requiring immediate medical intervention. Monitoring and dose adjustments are crucial, especially in patients with hepatic impairment, where metabolism may be altered.
- Additional Considerations
- Food Interaction: Food reduces oral absorption, decreasing peak plasma concentrations by 34% and extent by 24%, so it is recommended to take Voriconazole on an empty stomach, at least 1 hour before or after meals.
- Special Populations: Dose adjustments may be necessary for patients with liver dysfunction (e.g., reduce maintenance dose by half for mild to moderate impairment), and caution is advised in renal impairment for IV administration due to potential accumulation of the vehicle (sulfobutyl ether beta-cyclodextrin sodium). Safety and efficacy are not established for children under 2 years.
- Drug Interactions: Voriconazole is metabolized by hepatic cytochrome P450, leading to significant interactions with drugs like rifampin, carbamazepine, and certain protease inhibitors, which may necessitate dose adjustments or contraindications.