r/anhedonia
Personal Wiki
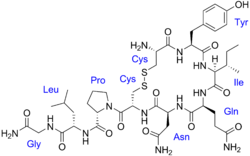
Oxytocin
- Pharmacological Actions
- Oxytocin's pharmacological actions are multifaceted, reflecting its therapeutic and physiological roles:
- Stimulation of Uterine Contractions: Oxytocin is renowned for inducing and strengthening uterine contractions, essential during labor and for managing postpartum hemorrhage. It activates oxytocin receptors on the myometrium, increasing intracellular calcium and enhancing contraction frequency and strength, regulated by a positive feedback loop during childbirth (source).
- Milk Ejection: It facilitates milk ejection during breastfeeding by stimulating the release of milk from mammary glands, crucial for lactation post-delivery.
- Behavioral and Social Effects: Research suggests oxytocin influences social cognition, pair bonding, maternal behavior, and fear conditioning. It is implicated in enhancing social interactions and has been explored for potential therapeutic uses in conditions like autism and anxiety, with receptors distributed in the brain stem and amygdala (source).
- Metabolic and Cardiovascular Effects: Oxytocin has pleiotropic effects, including impacts on metabolic functions and cardiovascular regulation, though these are less emphasized in clinical settings.
- The time course for these actions varies: uterine contractions and milk ejection effects are rapid, typically within minutes, while behavioral effects may have longer, less defined durations, often studied in hours to days for central effects.
- Half-Life
- The plasma half-life of oxytocin ranges from 1 to 6 minutes, with a noted decrease during late pregnancy and lactation, reflecting its rapid metabolism and clearance. This short half-life necessitates continuous or frequent administration for sustained effects, such as during labor induction (source).
- Bioavailabilities
- Bioavailability varies significantly by administration route, influenced by oxytocin's peptide nature and susceptibility to degradation:
- Parenteral (IV, IM): Administered intravenously or intramuscularly, oxytocin is fully bioavailable (100%), as it enters directly into systemic circulation, reaching steady-state plasma concentrations in approximately 40 minutes (source).
- Intranasal: Intranasal administration is effective for central nervous system effects, with evidence suggesting it crosses the blood-brain barrier, exhibiting psychoactive effects. However, specific bioavailability percentages are not consistently reported, though studies indicate central duration of at least 2.25 hours (source).
- Sublingual: Studies in male volunteers show sublingual bioavailability is very low, ranging from 0.007% to 0.07%, due to limited absorption through oral mucosa (source).
- Oral (Swallowed): Oral administration faces significant challenges due to degradation in the gastrointestinal tract by enzymes like pepsin. Research suggests bioavailability is extremely low, likely less than 1%, with one study noting a 200 IU tablet's effect equivalent to a 0.02 IU/min IV infusion, indicating negligible absorption without protective measures like proton pump inhibitors (source). Studies in mice with omeprazole pretreatment show increased plasma levels, but human data remain limited.
- Dosages
- Dosages are tailored to the clinical indication, with precise administration guided by patient response and monitoring:
- Labor Induction: Initiated at 0.5 to 1 milliunits per minute (mU/min) intravenously, titrated by increasing 1 to 2 mU/min every 30 to 60 minutes until a contraction pattern similar to normal labor is achieved, typically up to 6 mU/min, rarely exceeding 9 to 10 mU/min at term due to lower uterine sensitivity before term (source).
- Postpartum Hemorrhage: Administered as 10 units intramuscularly after placenta delivery, or 10 to 40 units added to 1000 mL of IV solution, infused at a rate to sustain uterine contraction and control atony, not exceeding 40 units total in the solution (source).
- Incomplete or Inevitable Abortion: Typically 10 to 20 mU/min IV, with a total dose not exceeding 30 units in 12 hours to mitigate risks like water intoxication (source).
- Safe Range, Minimum Effective Dose, Maximum Safe Dose, and LD50
- Safe Range: The safe dosage range is highly individualized, requiring continuous monitoring of uterine activity and fetal heart rate to prevent hyperstimulation and fetal distress. Adjustments are made based on clinical response, with guidelines suggesting not exceeding 10 mU/min for labor induction at term and limiting total doses for abortion to avoid water intoxication.
- Minimum Effective Dose: For labor induction, the minimum effective dose is approximately 0.5 mU/min IV, initiating contractions, with titration based on response.
- Maximum Safe Dose: There is no universal maximum, but clinical practice suggests rarely exceeding 9 to 10 mU/min for labor induction at term, and for postpartum hemorrhage, up to 40 units in IV solution. Prolonged high doses increase risks of adverse effects.
- LD50: Lethal dose 50% (LD50) data are derived from animal studies, with rats showing an LD50 of approximately 20.520 mg/kg and mice 514 mg/kg for systemic administration, indicating relatively low toxicity in animals. Human LD50 is not established due to ethical constraints, but clinical overdose risks include uterine hyperstimulation and water intoxication (source).
- When It Starts to Become Too Dangerous
- Oxytocin becomes dangerous when it leads to adverse effects such as uterine hyperstimulation, potentially causing fetal distress, or water intoxication from prolonged high doses due to its antidiuretic effect, leading to hyponatremia. Monitoring is critical, with discontinuation recommended if hyperactivity or fetal distress is observed, and oxygen administration may be necessary (source).
- Pharmacological Actions and Side Effect Mechanisms
- Oxytocin's primary pharmacological action is to bind to G-protein-coupled Oxytocin receptors in the myometrium, increasing intracellular calcium levels and triggering uterine contractions. This mechanism is essential for labor but can lead to hyperstimulation if doses are excessive, reducing placental blood flow and causing fetal distress. The antidiuretic effect, mediated by V2 receptors in the renal collecting ducts, promotes water reabsorption, which can result in water intoxication, especially with prolonged infusion and large fluid volumes, leading to hyponatremia, seizures, and coma in severe cases.
- Cardiovascular effects include vasodilation, which can cause hypotension, particularly with rapid intravenous administration, and may lead to arrhythmias. The risk of uterine rupture is heightened in scarred uteri due to pre-existing weaknesses, exacerbated by Oxytocin's strong contractile effects. For unscarred uteri, rupture is rare but can occur with prolonged or high-dose use, likely due to overstretching of the uterine wall.
- Incidence Data and Limitations
- Incidence rates for common side effects (e.g., tachycardia, nausea) are derived from drug information sources like Drugs.com, indicating a 1-10% range, which aligns with clinical trial data for similar medications. For rarer events like uterine rupture, specific studies provide estimates: in women with a scarred uterus undergoing TOLAC with Oxytocin, incidence is around 1-2% (source). However, exact frequencies for many side effects, such as water intoxication or neonatal jaundice, are not consistently reported, reflecting underreporting in clinical trials and the need for further research.
- Clinical Implications and Monitoring
- Given the potential for serious side effects, clinical guidelines emphasize careful monitoring during Oxytocin administration, including continuous fetal heart rate monitoring and maternal vital signs. The FDA has issued a "black box" warning for Pitocin due to its high-risk profile, highlighting the need for judicious use (source). Water intoxication, for instance, requires monitoring of fluid intake and sodium levels, while uterine rupture risk necessitates avoiding Oxytocin in high-risk cases like multiple prior cesareans.